When I got up this morning, trending on my Twitter feed was the news that the WWE (World Wrestling Entertainment) superstar, Roman Reigns (real name Joe Anoa’i), was in remission from leukaemia. In was in October 2018, in front of a packed arena, holding the Universal Championship belt, that he told the world that he needed to take time away to face the disease.
Just five months later he’s back and we should be celebrating this. But some people aren’t. Some wrestling fans think this is a work. Just to bring you inside the business a little, a work is an act that manipulates an audience in order to elicit a desired response. This is not a work. And my first feeling toward the people who were saying this was to scoop them up, slam them down on the canvas and cover them for the 1-2-3.
But I won’t. You see, there’s a fundamental flaw in all of this, Roman’s remission appears to be too good to be true. Looking great with all of his hair, five months after diagnosis doesn’t fit in with the traditional narrative of a blood cancer patient. Cancer doesn’t work like that, does it?
Actually, yes, some blood cancers do. I’ve had a similar type of blood cancer to Roman called chronic myeloid leukaemia (CML) for 11 years now. I take a small white tablet every morning called a tyrosine kinase inhibitor (TKI) and it puts my leukaemia back in its box on a molecular level. I’ve had bad days where I’ve felt tired or a bit sick but I’ve carried on. I work full time in education and haven’t taken a day off sick through anything related to the leukaemia. It took me about 9 months to reach a haematological level of remission, in that my blood looked OK. It took 6 years to get to a molecular level of remission and now my leukaemia is pretty much undetectable. I’ve never lost my hair and I’ve never had traditional chemotherapy.
You see where I’m going with this? Roman is an elite athlete and it might surprise you that I’m not. We’ve both fought our leukaemia in our own way and in our own timeframe. But there is one thing that I guarantee will annoy any leukaemia patient who is in remission, that’s someone saying, “well, you don’t look sick!” Right now, that’s happening online. Can’t we celebrate Roman looking great and happy or would we prefer him hooked up to a drip, pushed out in a wheelchair? That’s our traditional view and if our traditional view has been upended, it isn’t a lie.
The treatment that has given Roman and me our lives back was hailed in 2001 by Time Magazine as the magic bullet for cancer. Times are changing, we’re the trailblazers and millions of people are now living because of that little white tablet. They aren’t having devastating does of chemotherapy and in most cases, after taking the tablet they are able to go to work or smash someone around in a wrestling ring. It’s still not perfect, some people get side effects from the drugs but as the treatment improves, so will the quality of life.
We’re winning this battle and if we can win this one, we can win other battles against cancer. So take the time out to celebrate this, think of a world where we could treat cancer with a tablet; isn’t that what we’ve been wishing for? I’m living proof. Roman Reigns is living proof and so are millions of patients across the world.
But, let’s not forget, and Roman knows this all too well, leukaemia can relapse. We’re all living on a knife edge from appointment to appointment. My appointments are six months apart and I still get nervous, I’m sure that I always will. It’s a strange way to live…but it’s better than the alternative.
If Roman wants to make an even bigger difference he’ll tell his story. He’ll educate people, in detail, on the journey that he’s been through and he’ll tell them why, after five months of being diagnosed with blood cancer, he looks fantastic. Give people even more hope and help them understand that whilst we are a long way from winning the war, we are fighting back.
Please share this, it’s a great opportunity to educate people on blood cancer which is the third biggest cancer killer behind lung and bowel cancer in the UK.
Kris is 43 years old and lives in Kidderminster with his wife and young son. He is a trustee for Leukaemia Care and to celebrate his 10 years of diagnosis he raised £10,000 for the charity. If you are a wrestling fan (or just someone interested in this story) and want to get involved with the charity and raise money, please visit https://www.leukaemiacare.org.uk/support-and-information/latest-from-leukaemia-care/blog/wrestling-fundraising-ideas/
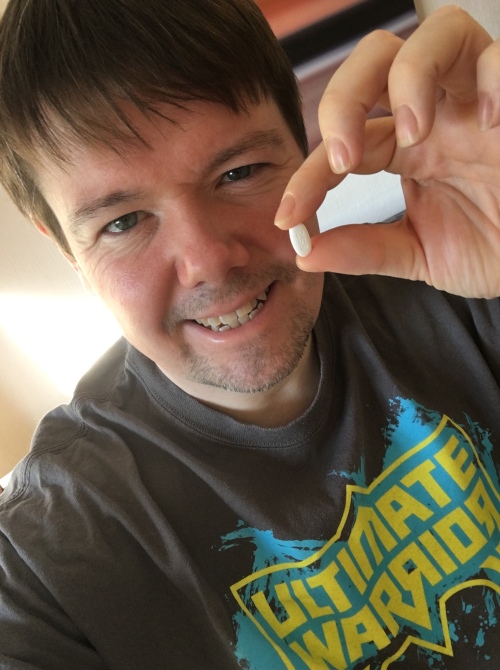
Kris holding his leukaemia treatment in tablet form.






